Free MCQ Questions
Question 1Posted on: Aug 20th 2020
21 year old male has one episode of syncope
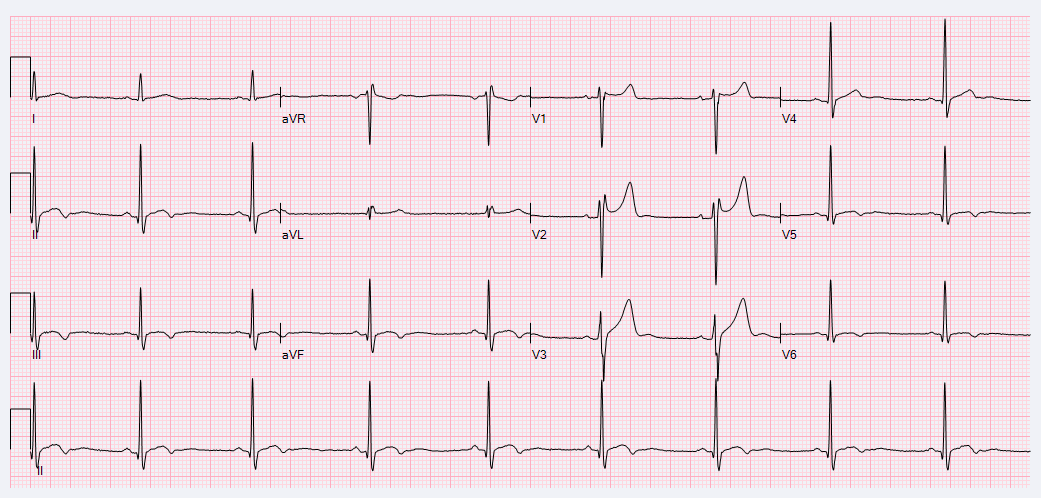
- Complete Right Bundle Branch Block
- Brugada Type 2
- Brugada Type 1
- Incomplete Right Bundle Branch Block
Show Answer
Answer: Choice 2: Brugada Type 2
Explanation:
Type I: Lead V1 has a “coved” ST segment elevation of at least 2 millimeters, followed by a negative T wave.
Type II: There is a “saddleback” appearance of the ST segment in lead V1 with ST segment elevation of at least 2 millimeters; this can be present in normal individuals as well.
Type III: Features of type I (coved) or type II (saddleback) with < 2 mm of ST segment elevation.
These ECG changes can be provoked in the electrophysiology lab by infusing procainamide.
The treatment for Brugada Syndrome is an ICD (implantable cardioverter defibrillator).
Brugada J, Campuzano O, Arbelo E, Sarquella-Brugada G, Brugada R. Present Status of Brugada Syndrome: JACC State-of-the-Art Review. J Am Coll Cardiol. 2018;72(9):1046-1059.
doi:10.1016/j.jacc.2018.06.037
Question 2Posted on: Jun 28th 2019
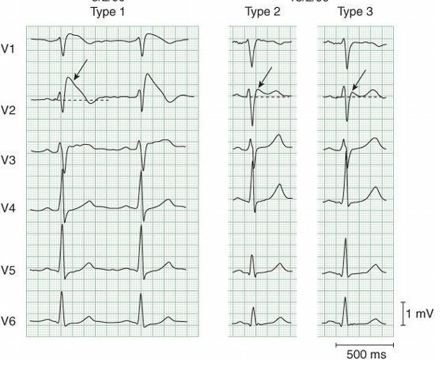
A 72 year old man tripped over his carpet at home and fell to the floor.
What does the CT scan of the head show ?
- Subarachnoid hemorrhage
- Intracerebral hemorrhages
- Hydrocephalus
- Cerebral contusions
- Subdural hematoma
Show Answer
Answer: Cerebral contusions
Explanation:
he patient suffered bifrontal and insular contusional hemorrhages which tend to grow over time.
https://www.henryford.com/physician-directory/m/mayer-stephan
Question 3Posted on: Jun 27th 2019
A 27-year-old man presents with fatigue but otherwise negative past medical history. The family history is negative for hematologic disorders
His WBC count is 700 per µl (normal, 3,400–10,000 per µl), neutrophils 250 per µl (normal, 1,800–6,800 per µl),
Hemoglobin 7.2 g/dl (normal, 13.6–17.5 g/dl), platelets 23,000 per µl (normal, 140,000–450,000 per µl), and absolute reticulocyte count 2 (normal, 24–100 per µl).
A bone marrow aspirate shows no spicules and a scant amount of mixed hematopoietic cells of normal morphology and a normal male karyotype.
The bone marrow biopsy is 2% cellular.
These findings are most compatible with which of the following?
- MDS
- Pure red blood aplasia due to parvovirus B19 infection
- Chronic idiopathic myelofibrosis
- Idiopathic aplastic anemia
Show Answer
Answer: Idiopathic aplastic anemia
Explanation:
A young man presents with pancytopenia and a hypocellular bone marrow. Since the bone marrow had an aspirate, this is not myelofibrosis (that would be a dry tap).
The normal morphology of hematopoietic cells in the bone marrow and the normal karyotype argue against MDS.
The lack of rash and fever argue against parvovirus B19, especially with this being pancytopenia and not isolated hypoproliferative anemia.
The best diagnosis is idiopathic aplastic anemia (d), especially with no family history to suggest an inherited bone marrow failure state.
Contributed by Lloyd Damon, MD Director of the adult Blood and Marrow Transplant and Hematologic Malignancies Program and Chief of the UCSF Hematology Clinic.
https://www.ucsfhealth.org/lloyd.damon
Question 4Posted on: Jun 26th 2019
A 71-year-old woman with well-controlled atrial fibrillation and a 60 pack-year smoking history develops weakness, fatigue, and intermittent headaches. She reports occasional cough productive of blood tinged sputum.
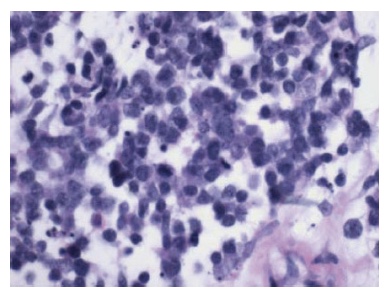
Laboratory studies reveal her sodium to be 121 mEq/L. Chest x-ray demonstrates a 5cm right hilar opacity with moderate right pleural effusion. Aggressive fluid restriction results in moderate improvement of hyponatremia. A representative H& E slide from bronchoscopic biopsy is shown in figure A. Thoracentesis yields similar findings.
What is the next step in the management of this patient.
- Treatment for pulmonary aspergillosis
- Treatment for chlamydia psitacci pneumonia
- Steroids for inflammatory lung disease
- Chemotherapy
- Surgery
Show Answer
Answer: Chemotherapy
Explanation:
Up to 10% of patients with SCLC will manifest signs and symptoms of inappropriately elevated anti-diuretic hormone which is secreted by tumor cells.
Osmolarity determination will show decreased serum osmolarity and hyperosmolar urine. Management of hyponatremia due to SIADH is water restriction and treatment of the underlying cause; in this case treatment directed towards SCLC.
Other paraneoplastic symptoms associated with SCLC include Eaton Lambert myasthenia syndrome, ectopic ACTH secretion, sensory neuropathy, and limbic encephalopathy.
Contributed by Scott Gettinger, MD Associate Professor Yale University https://www.yalecancercenter.org/patient/people/scott_gettinger.profile
Question 5Posted on: Jun 21st 2019
Which of the following clinical scenarios constitutes a contraindication to the initiation of beta-adrenergic receptor blockade in a patient with heart failure due to systolic dysfunction?
- A 46-year old outpatient with NYHA class III heart failure with a severely reduced ejection fraction (15%) and a blood pressure of 105/65mmHg.
- A 27-year old inpatient with newly diagnosed cardiomyopathy with no rales or edema on exam with an ejection fraction of 30%.
- An 86-year old outpatient with NYHA class II heart failure with an ejection fraction of 35%, a heart rate of 60 beats per minute, blood pressure 125/80 mmHg, and first degree atrioventricular block (PR interval is 240 msec).
- A 78-year old outpatient with class III heart failure with an ejection fraction of 25% and prior history of mild orthostasis with a beta-adrenergic receptor blocker.
- A 55-year old inpatient 12 hours post a large anterior myocardial infarction with an ejection fraction of 35% and systolic blood pressure of 88 mmHg on a low dose of dobutamine (2.5 mcg/kg/min).
Show Answer
Answer: A 55-year old inpatient 12 hours post a large anterior myocardial infarction with an ejection fraction of 35% and systolic blood pressure of 88 mmHg on a low dose of dobutamine (2.5 mcg/kg/min).
Explanation:
Initiation of beta-adrenergic receptor blockade for the treatment of heart failure is contraindicated when the patient is hypotensive and receiving treatment with a positive inotropic agent.
Beta-adrenergic receptor blockade should only be initiated or uptitrated in periods of clinical stability.
Potential contraindications to beta-adrenergic receptor blockade include symptomatic hypotension, symptomatic bradycardia, and greater than first degree heart block.
Choice 1 is incorrect as this patient has no described contraindication.
Choice 2 is incorrect as this patient has no described contraindication.
Choice 3 is incorrect as a heart rate of 60 is at the lower limits of the normal range and is not a contraindication to therapy, and first degree heart block is not a contraindication to therapy.
Choice 4 is incorrect as mild orthostatic symptoms are a common side effect of beta blockers, but not a contraindication to therapy.
Contributed by Dr Alex Reyentovitch, MD https://nyulangone.org/doctors/1588723662/alex-reyentovich … & Stuart Katz, MD @nyulangone
https://nyulangone.org/doctors/1306834478/stuart-d-katz … @nyuschoolofmed
Question 6Posted on: Jun 20th 2019
A 52 year old man with known alcohol abuse is brought to ER in stupor. He is vomiting and complains of vague abdominal pain.
On exam, BP 110/68, T 99, P 100. He is disheveled, neck is supple, and liver is palpable. No other findings are positive.
UA: pH 5, 6-10 WBC, 2-4 RBC, few granular casts and calcium oxalate crystals
Based on these findings and lab data below, The best explanation for his metabolic acidosis is:
- metabolic acidosis of renal failure
- salicylate intoxication
- ethylene glycol intoxication
- lactic acidosis
Show Answer
Answer: Ethylene glycol intoxication
Explanation:
This patient has high anion gap metabolic acidosis with appropriate respiratory compensation (expected pCO2 = 1.5 x HCO3 + 8 = 1.5 × 10 + 8 = 23 ± 2). Additionally, the osmolar gap is increased (24 = measured serum osmolality – calculated serum osmolality = 327- 301).
The conditions that cause high anion gap metabolic acidosis with high osmolar gap include ethylene glycol, methanol, propylene glycol, ethanol, and renal failure.
After accounting for the osmolar contribution of ethanol to the serum osmolality (11= ethanol concentration in mg/dL divided by 4.6), the osmolar gap still remains greater than 10. The presence of calcium oxalate crystals is strongly suggestive of ethylene glycol ingestion.
Mild lactic acidosis likely represents a laboratory artifact. The lactate analyzer mistakenly identifies glycolate as lactate because this metabolite of ethylene glycol bears a close structural resemblance to lactate.
Ketoacidosis is likely from alcoholic ketoacidosis. Modest acute kidney injury seen in this patient is not expected to cause metabolic acidosis of this severity. Furthermore, acute kidney injury does not elevate the osmolar gap.
Salicylate intoxication induces a mixed acid-base disorder with respiratory alkalosis and metabolic acidosis, the latter from lactic acidosis and ketoacidosis. The degree of lactic acidosis does not fully account for the increase in the anion gap.
Contributed by Aldo Peixoto, MD Professor and John J Chang, MD Assistant Professor
https://medicine.yale.edu/intmed/people/aldo_peixoto.profile
Question 7Posted on: Jun 19th 2019
Which of the following is an accepted indication for initiation of noninvasive positive pressure ventilation (NIPPV) with established evidence?
- Acute respiratory failure in immunocompromised patients
- Status asthmaticus while awaiting intravenous steroids to work
- Patients with severe burns to avoid further mucosal injury from endotracheal tube
- Patients with mild forms of acute respiratory distress syndrome
Show Answer
Answer: Acute respiratory failure in immunocompromised patients
Explanation:
Studies suggests that NIPPV is associated with decreased ICU mortality, intubation rate, and ICU length of stay among immunocompromised patients with acute respiratory failure, when compared to invasive mechanical ventilation as the first modality of ventilator support. These outcomes are probably a consequence of fewer nosocomial infections among patients given a trial of NIPPV before moving forth with invasive mechanical ventilation. Therefore option A is correct
In a very small study of 30 emergency department patients, the use of NIPPV in severe asthma exacerbation resulted in a favorable outcome. However, this has not been replicated in larger studies, and thus should not be considered standard of care – option B is thus incorrect.
Patients with severe burns and airway involvement typically get worse before they get better, and take a long time to recover. There are no studies to suggest a beneficial outcome with NIPPV use in this population. While there may be special scenarios where NIPPV might be tried, as a group, there are no studies to show that those with ARDS – even those with milder disease – would benefit from NIPPV
Contributed by Dr. Shyoko Honiden, http://M.Sc . M.D., is an Asst Prof of Medicine at the Yale School of Medicine & Dr Dr. Mark David Siegel, the Director of the Traditional Internal Medicine Residency at Yale. @HeartBobH @FutureDocs @StanfordDeptMed @UCSFHospitals
Question 8Posted on: Jun 18th 2019
A 35-year-old female presents to your clinic with excessive daytime fatigue, despite 8 hours of nightly sleep. She snores loudly and her bed partner has witnessed apneas. She is obese and also has asthma.
Her upper airway exam is very crowded, Modified Mallampati IV. Her nasal septum is deviated with near obstruction on the left.
You are concerned about sleep apnea. Which of the following screening tool can effectively rule in or out sleep apnea?
- Epworth Sleepiness Scale
- Berlin questionnaire.
- Overnight oximetry
- STOP-BANG
- None of the above
Show Answer
Answer: None of the above
Explanation:
There is no clinical model that accurately predicts disease severity in sleep apnea. Thus objective testing via a sleep study is required to determine disease absence or presence and severity.
The Epworth Sleepiness Scale is an 8 question scale used to measure the degree of daytime sleepiness. It asks subjects to rate, with increasing probability from 0--3 (0 = never, to 3 = very likely) their likelihood of falling asleep in 8 frequently encountered situations. It has been validated in SDB and can be useful to gage treatment response;
The Berlin Questionnaire is a 10-question test used to predict the presence of sleep apnea. The questionnaire refers to BMI, snoring, apneas, daytime sleepiness, drowsy driving frequency, and hypertension.
STOP-BANG, is a questionnaire focused on identifying SDB risk in the peri-operative population. The questionnaire borrows from Berlin, also incorporating information on age, neck circumference, and gender.
Overnight oximetry can be considered for screening of high risk patient groups. The test is not diagnostic for SDB and can be quite limited by false negative and false positive results.
Question 9Posted on: Jun 15th 2019
A 59-year-old female is in the office for the evaluation of hypothyroidism. She carries a diagnosis of Hashimoto’s thyroiditis made many years ago.
Her thyroid function has been stable on 125 µg of Levothyroxine daily for many years. However, she feels that she is having progressive fatigue for the past several months. Her appetite is decreased but she has gained 10 pounds despite reduced food intake and adequate exercise. She has also noticed that she is losing hair. In addition, her chronic constipation is getting worse, which she attributes to the addition of Calcium Carbonate tablets in the morning for her bone health. No other new medications were added. She has been using the same brand of Levothyroxine
In physical examination, her blood pressure was 134/80 mm Hg, heart beat was regular and the rate was 76/minute. She weighs 180 pounds and she is 64 inches tall. Her body mass index is 30.9 kg/m2. Eye examination demonstrates normal extraocular movements. There was no lid lag or proptosis. Thyroid examination reveals a small thyroid without any obvious nodule. Her skin is cool and dry to touch without obvious lesions. Her neurological exam is free of any focal findings. Bilateral reflexes are intact without any obvious delay. All other physical examination findings were unremarkable.
Laboratory. TSH: 8.1 uIu/mL (Reference: 0.5–4.2 uIu/mL) Total T4: 6.8 mcg/dL (Reference: 4.6–12.0 mcg/dL) Free T4: 1.0 ng/dL (Reference: 0.93–1.7 ng/dL)
Which of the following is the best next step in the management of her hypothyroidism?
- Patient is likely to have progression of hypothyroidism, a detail work up including TPO antibody, thyroglobulin, thyroglobulin antibody, thyroid ultrasound, RAIU, and thyroid scan are required to identify the possible cause for the worsening hypothyroidism
- This is likely to be secondary to drug-drug interaction. A careful review of the medication list and the method of intake are essential for the identification of the cause.
- Patient is likely to have malabsorption. She should undergo a gastrointestinal evaluation to identify the cause.
- Patient is likely to have progression of hypothyroidism. This should be managed by immediately increasing her dose of Levothyroxine to 150 mcg, daily
- Patient is not having disease progression. Her significant weight gain is likely the cause responsible for the increased demand of Levothyroxine. Based on her body weight of 180 pounds (81.65 kg), the daily requirement of Levothyroxine is 130 µg
Show Answer
Answer: This is likely to be secondary to drug-drug interaction. A careful review of the medication list and the method of intake are essential for the identification of the cause.
Explanation:
This is a common scenario seen in the office management of hypothyroidism. A careful review of medical history and medication list can sometimes identify the causes responsible for the increasing demand of Levothyroxine dose. In this case, the patient has added Calcium Carbonate tablets in the morning. Unfortunately, calcium carbonate has extensive interaction with Levothyroxine and can severely compromise the absorption of the later. Therefore, the best next step of action will be to change the morning calcium carbonate to be at least one hour after Levothyroxine to minimize the compromised absorption of the thyroid hormone. There is no need to change the dose of Levothyroxine as yet since an obvious underlying cause can be identified and should be removed. As a follow up, TSH should be re-checked in ~6 to 8 weeks with the aim to correct it into normal reference range. It should be noted that T4 monotherapy is the preferred treatment for hypothyroidism. Levothyroxine is known to have extensive drug-drug and drug-food interaction. Therefore, it is recommended that it should be taken in early morning in empty stomach with water only. It should be separated from any other oral medications or food for ~1 hour. In addition, the bioavailability of different preparations of thyroid hormone is different and whenever a brand is changed, TSH should be re-measured in 6 to 8 weeks to ensure the stability of thyroid function
Choice a is incorrect. Patient is known to have Hashimoto’s thyroiditis, which is the most likely cause for her hypothyroidism. Her TPO and thyroglobulin antibodies are all likely to be positive. Repeated measurements of these antibodies are likely to be low yield in the work up of her worsening hypothyroidism. In addition, RAIU and thyroid scan are unlikely to identify the cause of her increasing demand of Levothyroxine.
Choice c is incorrect. There is no indication that patient is having a gastrointestinal issue at this time that warrants an investigation.
Choice d is incorrect. All the obvious underlying cause should be addressed before simply increasing the dose of the medication.
Choice e is incorrect. The weight gain of the patient is likely secondary to the worsening hypothyroidism. Simply increasing Levothyroxine dose may or may not be able to correct her hypothyroidism unless the underlying cause was corrected. Besides, the estimation of Levothyroxine dose is based on body lean mass instead of the actual weight. Increasing her Levothyroxine from 125 to 130 µg daily is unlikely to be the best choice.
James V. Hennessey, MD is Director of Clinical Endocrinology at Beth Israel Deaconess Medical Center in Boston, MA. He is an Associate Professor of Medicine at the Harvard medical School.
Question 10Posted on: Jun 14th 2019
A 27 year old man presents complaining of a rash. He states that he noticed a tick attached to his right arm approximately 1 week ago, and yesterday at that site he noted onset of a red, painless lesion that has grown larger over the last 24 hours (Photo).
He denies fevers but states he has felt more fatigued than usual. He has not travelled outside of his native state of Missouri.
What is the most appropriate next test?

- Serologies for B. burgdorferi
- Complete blood count (CBC)
- Serologies for R rickettsii
- No additional testing indicated
- Serologies for E. chaffeensis
Show Answer
Answer: No additional testing indicated
Explanation:
The skin lesion has an area of central erythema with clearing, suggestive of a target or bulls-eye appearance. This, coupled with the recent tick bite at the site and the history of enlarging size is diagnostic of an erythema migrans skin lesion, which may be seen either with Lyme disease or with Southern tick associated rash illness (STARI).
Although the skin findings for these two diseases are identical, they occur in distinct geographic regions. B. burgdorferi, the etiologic agent of Lyme disease, is found in ticks endemic to the Northeast and upper Midwest United States.
The etiologic agent of STARI is not known, but the disease is transmitted by the lone star tick, with is found through the Southeast and South Central regions, including Missouri. Regardless, laboratory confirmation is not needed for Lyme disease when a classic erythema migrans rash is present, as antibodies may not yet have developed at this early stage
While human monocytic ehrlichiois (HME), caused by E chaffeensis, and Rocky Mountain spotted fever (RMSF), caused by R. rickettsii have both been reported in patients from Missouri, neither disease is associated with an erythema migrans skin lesion.
Hematologic abnormalities are frequent with both HME and RMSF, but are not present with STARI.
https://medicine.mc.vanderbilt.edu/person/karen-c-bloch-mdmph-fidsa
Question 11Posted on: Jun 13th 2019
A 42-year-old man presents to the ER after being hit by a vehicle. He says the vehicle hit his right leg and he now has both foot pain and weakness.
On examination he has 0/5 power in his right tibialis anterior and extensor hallicus longus. He has 3/5 power in his right foot evertors. Foot inversion is 5/5. He has decreased sensation to pinprick on the dorsum of the right foot especially in the web space between the first and second toes.
What is the best localization of this injury?
- L5 radiculopathy
- Peroneal nerve
- Sciatic nerve
- Tibial nerve
- Femoral nerve
Show Answer
Answer: Peroneal nerve
Explanation:
The pattern of weakness and sensory loss fits best with injury to the peroneal nerve.
A peroneal neuropathy should be distinguished from a L5 radiculopathy by testing foot inversion. Foot inversion is performed by the posterior tibialis muscle which is supplied by the tibial nerve through the L5 root. Thus, an L5 radiculopathy will cause weakness of foot inversion in addition to foot dorsiflexion, but a peroneal neuropathy will have weakness in foot dorsiflexion, but spare foot inversion.
The peroneal nerve has both a deep and superficial branch.
The deep peroneal nerve supplies the tibialis anterior, extensor hallucis longus and supplies sensation in the webspace between the first and second toe.
The superficial peroneal nerve supplies the foot evertors (peroneus) and sensation to the dorsal aspect of the foot.
The sciatic nerve divides into both the tibial and peroneal nerve.
The femoral nerve supplies the quadriceps and iliopsoas muscles.
https://weillcornell.org/josafdieh
Question 12Posted on: Jun 11th 2019
A 23 year old woman attends clinic for her pre-college physical. Her history is notable for frequent episodes of sinusitis and several years of loose bowel movements. She denies urgency, bleeding, or incontinence, and is having 3 to 4 loose stools a day. She was told she had “Irritable Bowel” by her pediatrician.
Laboratory studies are notable for a protein level of 4.8 g/dL, and very low quantitative immunoglobulins for serum IgG, IgM and IgA. Celiac serologies and stool studies were negative.
You refer her for an EGD, which showed “duodenal scalloping”, and the biopsy report notes “villous blunting with a lack of plasma cells”.
What is the likely diagnosis?
- Sero-negative celiac disease
- Lymphoma
- Common variable immunodeficiency syndrome
- Burton's agammaglobulinemia
Show Answer
Answer: Common variable immunodeficiency syndrome
Explanation:
Common variable immunodeficiency syndrome is characterized by frequent sinus infections and diarrhea, in the setting of normal celiac serology and absent quantitative immunoglobulins.
Duodenal biopsies will show villous atrophy and a lack of plasma cells.
Patients with celiac disease can have a false negative TTG test in the setting of immunoglobulin deficiency, but an absence of plasma cells is not a feature of celiac disease on biopsy.
Lymphoma would have characteristics features on histology, and
Burton's agammaglubulinemia will not have duodenal abnormalities.
Contributed by Drs Maggie Ham, MD and Alan C Moss, MD, Harvard Medical School
Question 13Posted on: Jun 7th 2019
A patient presents with a large right pleural effusion. A mass is seen in the apex of the lung and she has cervical lymphadenopathy.
A thoracentesis is performed and the following values are observed. . • Cell count: 10,000 WBC’s, 90% lymphocytes, 5% neutrophils • Pleural fluid LDH (U/L): 600 • Serum LDH (U/L): 200 • Pleural fluid protein (g/L): 4.3 • Serum protein (/L): 5.5 • Pleural fluid glucose: 50 mg/dl
Which of the following is true?
- This transudative effusion is likely caused by heart failure from chemotherapy for lung cancer.
- This transudative effusion is likely due to fluid resuscitation provided by treating tumor lysis syndrome.
- This exudative effusion is likely due to metastatic lung cancer.
- This exudative effusion is likely due to tuberculosis
- There is not enough information to determine if this effusion is a transudate or exudate.
Show Answer
Answer: This exudative effusion is likely due to metastatic lung cancer.
Explanation:
This is an exudative effusion as determined by Light's criteria. Although only 1 criteria is required, this patient's pleural fluid LDH to serum LDH ratio is >0.6 and the pleural fluid protein to serum protein ratio is > 0.5. She also has a lung mass and history of tobacco use. All of these suggest a malignant pleural effusion and advanced lung cancer
Contributed by Dr Jonathan Puchlaski, MD
Associate Professor of Internal Medicine (Pulmonary, Critical Care and Sleep Medicine)
Director, Interventional Pulmonology
Director, Interventional Pulmonary Fellowship
https://medicine.yale.edu/intmed/people/jonathan_puchalski.profile
Question 14Posted on: Apr 13th 2019
An unconscious 18-year-old male is brought to the emergency department via ambulance.
The report given by the paramedics was that his mother found him outdoors and unresponsive.
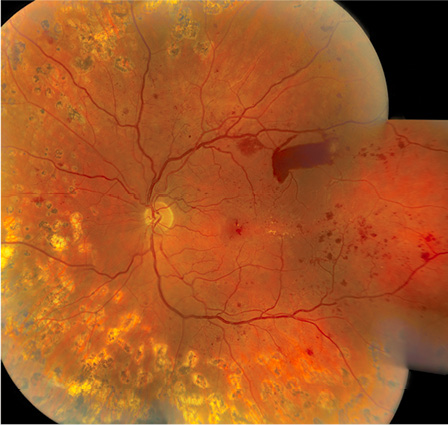
An examination of his fundus reveals .(Photograph courtesy of Yasha Modi M.D., Bascom Palmer Eye Institute.)
Which test should be performed immediately?
- Carotid Ultrasound
- HIV antibody Testing
- CT head
- Blood Glucose
Show Answer
Answer: Blood Glucose
Explanation:
DKA is an acute, major, life-threatening complication of diabetes, which leads to profound dehydration, acidosis, and electrolyte disturbances.
Prompt diagnosis and treatment is lifesaving. The clinician can perform a fingerstick glucose test while waiting for the serum chemistry panel.
It is typically characterized by hyperglycemia over 300 mg/dL. Approximately 8,000 eyes become blind yearly because of diabetes.
from: Galor A, Goldhardt R. Ophthalmology for the Internist in Baliga's Textbook of Internal Medicine: An Intensive Board Review Book with 1480 Multiple Choice Questions
Question 15Posted on: Apr 13th 2019
A study wishes to assess birth characteristics in a population. Which of the following variable types would be used to classify the type of delivery where delivery categories are labeled as: cesarean, natural, or induced?
- Discrete
- Continuous
- Ordinal
- Nominal
- Dichotomous
Show Answer
Answer: Nominal
Explanation:
Since the variable in question is broken into three naming categories that do not have any rank or order associated with them, the variable would be a nominal variable.
Contributed by Donna Windish, MD, Associate Professor of Medicine, Department of Internal Medicine at Yale University School of Medicine.
https://medicine.yale.edu/intmed/people/donna_windish.profile
Question 16Posted on: Apr 10th 2019
A 44-year-old woman is hospitalized after an open cholecystecomy complicated by post-operative fevers. She has been on antibiotics for three days.
You are consulted to evaluate a new rash. The patient is complaining of a pruritic eruption on her abdomen, which was first noted on post-operative day 2. She has no known drug allergies.
Physical examination is notable for eczematous, edematous plaques around the surgical wound.
Her medications are notable for: topical neomycin, ampicillin/sulbactam, morphine sulfate, subcutaneous heparin, and colace.
What is the most likely culprit for this eruption?
- Neomycin
- Ampicillin
- Sulbactam
- Morphine
Show Answer
Answer: Neomycin
Explanation:
The eczematous eruption limited to the surgical site suggests a focal or local cause of the rash.
Typical systemic drug eruptions are characterized by a morbilliform eruption, consisting of erythematous blanching macules and fine papules, usually on the trunk, flanks, upper inner arms, or accentuated at sites of pressure, such as the lower back in supine patients and around the elastic bands of clothing or pads.
An eczematous eruption, localized to a single site, is suggestive of a topical culprit. In this case, the patient is receiving neomycin to the surgical wound; neomycin is a common cause of allergic contact dermatitis, and in this case is the most likely culprit.
Rosenbach M, Micheletti R. A Practical Approach To The Diagnosis And Treatment Of Urticaria in Baliga's Textbook of Internal Medicine: An Intensive Board Review Book with 1480 Multiple Choice Questions
Question 17Posted on: Mar 27th 2019
A 20-year-old woman presents with pruritus localized to the axillae after using a new deodorant. In order to avoid striae formation, which of the following would be the best treatment option this patient?
- Fluocinonide 0.05% cream
- Capsaicin cream
- Pramoxine lotion
- Pimecrolimus
Show Answer
Answer: Pimecrolimus
Explanation:
This patient likely has allergic contact dermatitis. Of the available answers, pimecrolimus is the best one because it shares anti-inflammatory properties with topical corticosteroids but without the concerns regarding atrophy and hypopigmentation.
Fluocinonide is a potent topical corticosteroid and its use in intertriginous areas should be avoided.
While the topical neuromodulators capsaicin and pramoxine sometimes improve localized pruritus, neither one will affect the inflammation present in allergic contact dermatitis.
Question 18Posted on: Mar 27th 2019
A 50-year-old man with hypertension is scheduled to undergo posterior lumbar spinal fusion.
Which of the following findings on his preoperative evaluation should prompt delay or cancellation of the planned surgery?
- Frequent premature atrial complexes on ECG
- Myocardial infarction one year ago, treated with thrombolysis
- Atrial fibrillation with normal ventricular rate
- New complaint of dyspnea and a finding of a third heart sound
- Baseline serum creatinine of 2.1 mg/dL
Show Answer
Answer: New complaint of dyspnea and a finding of a third heart sound
Explanation:
Patients should not undergo elective surgery if they have severe or decompensated cardiac disease that requires immediate evaluation and treatment regardless of the upcoming operation. The findings of dyspnea and a third heart sound suggest decompensated heart failure, which should be addressed prior to surgery. Atrial ectopy on ECG, remote myocardial infarction, rate-controlled atrial fibrillation, and stable chronic kidney disease do not require urgent management and are not contraindications to surgery.
Cheng HQ. Perioperative Medicine. in Baliga RR (editor). Baliga's Textbook of Internal Medicine: An Intensive Board Review Book with 1480 Multiple Choice Questions, Blendon-Miller, An imprint of MasterMedFacts LLC
Question 19Posted on: Mar 25th 2019
A 38-year-old Caucasian woman with a history of polysubstance abuse since her teens is admitted with an extensive, painful purpuric eruption.
She has a history of positive serology for hepatitis B and C but is HIV negative. She first developed painful purpura involving the arms, thighs, legs, and ears 2 weeks previously and was admitted to another hospital but signed out 2 days later against medical advice. Workup there included positive HBsAb, negative HbsAg, positive HCV antibody, positive ANA 1:80, negative rheumatoid factor. A skin biopsy showed intravascular fibrin deposition. She denied fever, chills, or recent drug use.
On physical examination there was extensive retiform (angulated) purpura of the arms, thighs, legs and purpura of the ears (Figure 62). Her CBC was remarkable for neutropenia with an absolute neutrophil count of 1020 per cubic millimeter. Antineutrophil cytoplasmic antibody testing (ANCA) was positive for p-ANCA and c-ANCA, and an enzyme-linked immunosorbent assay revealed a proteinase-3 antibody titer of 1:160.
Which test should be done first to guide subsequent workup?

- ANCA
- Cryoglobulins
- Protein C and Protein S levels
- Urine toxicology
Show Answer
Answer: Urine toxicology
Explanation:
The patient described has severe retiform (angulated) purpura associated with purpura and necrosis of the skin of the ears. This is a typical presentation of thrombotic vasculopathy caused by levamisole-adulterated cocaine. This diagnosis would be suggested by the presence of cocaine in the urine. Antineutrophil cytoplasmic antibodies and ANA are commonly positive in this condition. The treatment is to discontinue cocaine and institute supportive measures. A plastic surgery consult should be obtained.
From Chismar LA, Rudikoff D. Approach to a Patient with Dermatologic Disease in Baliga RR (editor). Textbook of Internal Medicine:An Intensive Board Review Book with 1480 Multiple Choice Questions.
Question 20Posted on: Jan 23rd 2019
Which of the following is characteristic of asbestosis?
(Contributed by:
Ware G. Kuschner, MD is Professor of Medicine at Stanford University and Chief of the Pulmonary Section at the Veterans Affairs Palo Alto Health Care System, Palo Alto, California &
Paul D. Blanc, MD is Professor of Medicine and holds the Endowed Chair in Occupational and Environmental Medicine at the University of California San Francisco)
- Lower Lung Zone Predominance
- Innumerable pulmonary rounded radiographic opacities less than 10 mm
- “Egg shell” calcification affecting the hilar lymph nodes
- 3 – 8 year routine latency from onset of exposure to development of disease
- Virtually always found among individuals who develop malignant pleural mesothelioma
Show Answer
Answer: Choice 1: Lower Lung Zone Predominance
Explanation:
Asbestosis is a fibrotic lung disease caused by the inhalation of asbestos. It is characterized by reticular radiographic abnormalities and stacked cysts (“honeycombing”) in a sub-pleural distribution, typically involving the lower lobes of the lung initially.
Exposure settings associated with asbestosis have included asbestos mining, ship building, and asbestos textile manufacturing. A latency period of approximately 20 years or more between initial exposure and the development of clinically significant disease is typical. Individuals who develop malignant pleural mesothelioma do not necessarily exhibit asbestosis.
Silicosis is a diffuse parenchymal nodular lung disease that results from the inhalation of silicon dioxide (silica). The most common form of silicosis is chronic simple silicosis, which typically presents after 10 years of exposure to silica dust and results in small nodules, typically affecting the upper lung zones first. A subset of patients with silicosis will exhibit calcification of hilar lymph nodes - “egg shell calcification”.
Question 21Posted on: Dec 29th 2018
A 32-year-old woman reports her last menstrual period was 7.5 months ago. She had menarche at age 12 and menses every 28-30 days until one year ago, when she missed a period. She subsequently had 2 more periods and then nothing. She is nulliparous and reports condom use for contraception. She reports headaches daily, but attributed that to job stress. She takes no medications.
A home pregnancy test is negative. Laboratory testing revealed a negative HCG, normal TSH (1.2 mIU/mL), FSH 2.3 mIU/mL, LH 3.5 mIU/mL, estradiol < 20 ng/mL, and prolactin 42 ng/dL.
What is the next step in evaluation?
Contributed Drs Sara Divall, MD & Adrian Sandra Dobs, MD, MHS, Professor of Medicine at the Johns Hopkins University
https://www.hopkinsmedicine.org/profiles/results/directory/profile/0000716/adrian-dobs
- Refer to Neurosurgery for evaluation
- Obtain MRI of the brain and pituitary
- Start dopamine agonist therapy
- Repeat prolactin level
Show Answer
Answer: Choice 4: Repeat prolactin level
Explanation:
Prolactin level can be elevated by the stress of phlebotomy, recent breast or nipple manipulation (i.e. after a physical exam of breast tissue), medications, or sleep.
Verification of the elevation in prolactin should occur prior to proceeding with imaging. If fear of phlebotomy is severe, the stress of phlebotomy can be diminished by inserting an indwelling catheter, waiting 15–30 minutes, and then drawing the blood off the catheter
Question 22Posted on: Dec 14th 2018
A 58-year old chronic smoker (10-pack years) with COPD is readmitted to hospital. Her post-bronchodilator ratio of FEV1 to FVC is 0.69 with an FEV1 below 80% predicted. Which one of the following approaches is most likely to improve her outcomes?
- Self-administration of an antibiotic on flare-up of COPD using an action plan (chosen in consultation with the primary care physician) with instructions to initiate treatment within 48 hours after onset of exacerbation symptoms
- Self-administration of an oral steroid on flare-up of COPD using an action plan (chosen in consultation with the primary care physician) with instructions to initiate treatment within 48 hours after onset of exacerbation symptoms
- Transitional care support during hospitalization and following discharge (including inhaler education, smoking cessation, breathing techniques and developing an action plan to address signs and symptoms of exacerbations) and long-term self-management.
- Shared management between COPD specialists and primary care physicians
- Low-Dose Theophylline
Show Answer
Answer: Choice 3
Explanation:
Self-administration of antibiotics or steroids during acute exacerbations has been shown to increase mortality (Annals of Internal Medicine 2012;156(10):673-683). No benefit has been shown with co-management between COPD specialists and primary care physicians (Cochrane Database Syst Rev. 2007;3:CD004910). Low-dose theophylline, compared with placebo, has no effect of reducing the mean number of exacerbations among patients with COPD (JAMA 2018;320(15):1548-1559). A recent study from Johns Hopkins has demonstrated that a combination of transitional care support by COPD nurses (during hospital stay and 3-months after discharge) and long-term management can improve outcomes in COPD patients ( Rinne ST, Lindenauer PK, Au DH. Intensive Intervention to Improve Outcomes for Patients With COPD. JAMA 2018;320:2335-2343).
Question 23Posted on: Dec 12th 2018
A 73-year-old woman with hypertension and atrial fibrillation who lives in a skilled nursing facility develops delirium. A urinalysis reveals 105 WBC. Trimethoprim/Sulfa 1 DS PO BID is prescribed by telephone. Three days later, the patient presents to the emergency department with grossly heme positive black stool and is found to have a hematocrit of 21. Her INR is >7.5. On detailed review of the patient record the provider realizes she is also on warfarin. He states he was not aware that the patient was anti-coagulated. What is the adverse event in this case?
- The patient’s delirium
- The patient’s urinary tract infection
- The patient’s gastrointestinal bleed
- The patient’s supratherapeuticINR
Show Answer
Answer: 3: The patient's gastrointestinal bleed
Explanation:
Though the patient suffered from a UTI and delirium, from the details in the case these are not related to specific actions or processes of care. The gastrointestinal bleed is harm that she has suffered as a result of a supratherapeuticINR. Choice d is not correct as it does not describe harm per se. Contributed by Dr. Anjala V. Tess, MD is an Associate Chair for Education in the Department of Medicine at Beth Israel Deaconess Medical Center (BIDMC), Director of QI and Safety for GME at BIDMC, and an Associate Professor in Medicine at Harvard Medical School and Dr. Eric J. Alper, MD, FACP, SFHM is Professor of Medicine, UMass Medical School.
Question 24Posted on: Dec 6th 2018
A 71-year old male patient with chronic hepatitis C genotype 1b of six years duration was seen in the hepatology clinic. He drank a small glass of red wine everyday for 20 years. He had hepatitis A when he was 15 years old. Clinically he had no symptoms or signs of liver disease. Hemoglobin 12.2 g/dL, white blood count 7.9 x 103/ µl, platelet count 225 x 103/ µl, creatinine 1.0 mg/dL, total bilirubin 0.9 mg/dL, alanine aminotransferase 31 U/L, aspartate aminotransferase 27 U/L, alkaline phosphatase 48 U/L, albumin 3.9 g/dL. His hepatitis C was successfully treated (defined as no detectable HCV RNA 12 weeks after treatment) with combination therapy of simprevir (Olysio) and sofosbuvir (Sovaldi) for three months duration. Ultrasound of the liver showed no nodularity or signs of cirrhosis. His liver stiffness measurement (LSM), using vibration-controlled transient elastography (VCTE), was 21 kPa. The most likely diagnosis is
- Alcoholic liver disease
- Non-alcoholic fatty liver disease
- Cirrhosis due to chronic hepatitis C
- Normal liver
- Cirrhosis ruled out
Show Answer
Answer: C
Explanation:
Liver stiffness measurements (LSM) of 21 kPa suggests cirrhosis—it is greater than diagnostic threshold for cirrhosis which is 12.5 kPa (where the specificity is >94%) [1]. Area under the receiver operating curves, for cirrhosis, range from 0.93 to 0.99. VTCE is better at diagnosing cirrhosis than staging cirrhosis. The most common cause of cirrhosis and end-stage liver disease among adults awaiting hepatic transplantation, in the US, is chronic hepatitis C (35%), followed by alcoholic liver disease (18%) and non-alcoholic fatty liver disease (16%) [2]. He drinks in moderation so it is unlikely to cause alcoholic liver disease 1. Mueller S, Sandrin L. Liver stiffness: a novel parameter for the diagnosis of liver disease. Hepat Med 2010; 2: 49-67. 2. Wong RJ, Aguilar M, Cheung R, et al. Nonalcoholic steatohepatitis is the second leading etiology of liver disease among adults awaiting liver transplantation in the United States. Gastroenterology 2015; 148(3): 547-55.
Question 25Posted on: Nov 28th 2018
A 46-year-old homeless man is brought into the emergency department after being found unresponsive in a park. He is minimally responsive to sternal rub, and vomitus is noted on his shirt. His pulse oximetry reads 89% saturation on room air, and an ABG is drawn. The result is reported as 7.22/65/60. What is the most likely reason for this patient’s hypoxemia? Authored by Drs Shyoko Honiden, MD & Mark Siegel, MD, Yale University https://medicine.yale.edu/intmed/pulmonary/about/mark_siegel.profile
- V/Q mismatch due to aspiration pneumonitis
- Alveolar hypoventilation due to drug overdose
- Impairment in diffusion due to underlying interstitial disease
- Shunt physiology due to hepatopulmonary syndrome from alcoholic cirrhosis
Show Answer
Answer: Choice 2
Explanation:
The most likely reason for this patient’s hypoxemia is alveolar hypoventilation. Working thorough the alveolar gas equation, the PAO2 = FIO2(Patm-PH2O) – PaCO2/0.8. Assuming that the patient is on room air at sea level, PAO2 = 0.21(760–47) –65/0.8, which works out to be ~68.5mmHg. If you then subtract the measured PaO2 of 60mmHg, the alveolar to arterial (A-a) oxygen gradient comes out at 8.5 mmHg which is NORMAL. Hypoxemia related to V/Q mismatch, diffusion impairment, as well as shunts result in an elevated A-a gradient. Thus, alveolar hypoventilation, in this case most likely due to drug overdose, is the likely explanation. Contributed by Drs Shyoko Honiden and Mark Siegel, MD, Yale University https://medicine.yale.edu/intmed/pulmonary/about/mark_siegel.profile
Question 26Posted on: Nov 26th 2018
Researchers want to assess the mean change in the American Urological Association Symptom Index score (rated on a scale of 0 to 35) comparing saw palmetto versus placebo. Which of the following differences in scores would yield a statistically significant change? Contributed by Donna Windish, MD, Associate Program Director for the Yale Primary Care Internal Medicine Residency & Associate Professor, Yale University
- -1.68 (95% CI, -2.37 to 0.01)
- -1.90 (95% CI, -2.49 to -0.37)
- -1.45 (95%CI, -2.56 to 1.50)
- 0.50 (95% CI, -0.29 to 0.90)
Show Answer
Answer: Choice 2
Explanation:
Since the question is assessing a change (difference) in score, any confidence interval that contains the value of “0” would not be considered statistically significant. This leaves answer “2” as the only statistically significant result. (more details in the book chapter)
